Constipation
from a Functional Medicine Perspective
Constipation is one of the most common digestive complaints, yet it’s often misunderstood and oversimplified. In functional medicine, constipation isn’t just about infrequent bowel movements; it’s a sign that something deeper in the body is out of balance. Addressing it means identifying the root cause and restoring optimal digestive, nervous system, and detox function.
Understanding Constipation Beyond the Surface
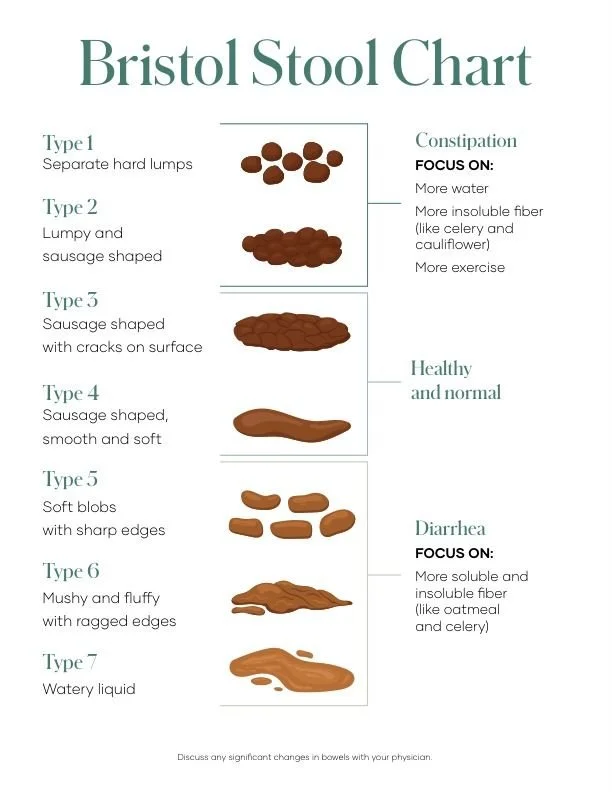
Clinically, constipation is defined as having fewer than three bowel movements per week, hard or difficult-to-pass stools, or a persistent feeling of incomplete evacuation. However, in functional medicine, we see it as a communication signal from the gut, pointing to sluggish motility, microbial imbalance, or impaired detoxification.
Chronic constipation can lead to toxin reabsorption, hormonal imbalance (especially estrogen dominance), dysbiosis, bloating, fatigue, and even skin issues. The goal is not just symptom relief but restoring the natural rhythm of elimination.
Root Causes of Constipation
Constipation is rarely caused by one single factor. Some of the most common underlying contributors include:
Gut dysbiosis (imbalanced gut bacteria)
Low stomach acid or bile flow
Dehydration
Insufficient dietary fiber or fat intake
Magnesium or electrolyte deficiency
Chronic stress and vagal nerve dysfunction
Thyroid dysfunction (especially hypothyroidism)
Medication side effects (e.g., antidepressants, iron supplements, opioids)
Functional Medicine Strategies for Relief
1. Hydration & Electrolyte Balance
Start with the basics: water and minerals. Hydration keeps stool soft and supports colon motility. Aim for half your body weight (in ounces) of filtered water daily, and include electrolytes from sources like coconut water, sea salt, or mineral drops.
Click here for electrolyte blends I like !!
2. Optimize Fiber Intake
To encourage healthy, regular bowel movements, start adding chia seeds, ground flaxseeds, kiwi, dragon fruit, aloe juice, and warm liquids into your daily routine. These foods help keep the digestive system hydrated and moving smoothly.
It’s important to remember that not all fiber is the same. A mix of soluble fiber, found in chia seeds, flaxseeds, psyllium husk, apples, oats, and sweet potatoes, and insoluble fiber from leafy greens, celery, carrots, cucumbers, and zucchini works best. Soluble fiber helps form a gel-like consistency that softens stool, while insoluble fiber adds bulk and promotes movement through the intestines.
If your digestion is on the sensitive side or you’re managing IBS, you may do better with low-FODMAP fibers such as oats, chia seeds, flaxseeds, carrots, and spinach. You can also support regularity by including magnesium-rich foods (like avocado, pumpkin seeds, and leafy greens), healthy fats (such as olive oil and coconut oil), and fermented foods (like sauerkraut, kefir, or coconut yogurt). Together, these foods nurture your gut microbiome and help your body maintain natural rhythm and balance.
Click here for fiber blends I like !!
3. Support Bile Flow and Digestive Function
Healthy bile flow is essential for fat digestion and bowel regularity. Support the liver and gallbladder with foods like beets, dandelion greens, artichokes, and lemon water. Digestive bitters or gentle bile-supporting supplements can also help stimulate peristalsis.
Click here for my favorite digestive enzyme blends !!
4. Restore the Gut Microbiome
A healthy microbiome regulates motility through short-chain fatty acid (SCFA) production. Incorporate probiotic-rich foods such as sauerkraut, kefir (dairy-free if needed), and fermented vegetables. For those with dysbiosis or overgrowth, targeted antimicrobial protocols may be necessary under practitioner guidance.
5. Relax the Nervous System
The gut and brain are deeply connected. Chronic stress shuts down the “rest and digest” state, slowing motility. Techniques such as deep breathing, vagus nerve stimulation, meditation, yoga, or gentle abdominal massage can help reestablish parasympathetic tone.
NOTE* Undereating and overexercising can all slow digestion. When the body feels undernourished or overworked, it shifts into “survival mode,” diverting energy away from digestion to prioritize vital organs. This reduces stomach acid, slows gut motility, and can lead to constipation. Over time, this stress response can throw off hormones like cortisol and thyroid function, both of which play key roles in regular bowel movements. Nourishing your body adequately, resting, and managing stress are just as important for healthy digestion as fiber and hydration !!!!!
Click here for my favorite ways to destress
Click here for my favorite colon massage. You can try massaging castor oil in your belly button, too.
6. Consider Natural Supports
Magnesium citrate or glycinate: Promotes relaxation and motility.
Castor oil packs: Encourage lymphatic flow and gentle detoxification. Click here to learn more
Aloe vera juice or triphala: Can naturally support bowel movement and tissue repair.
When to Seek Professional Support
If constipation persists longer than a few weeks, is accompanied by blood in the stool, significant pain, or unexplained weight loss, it’s important to consult a healthcare provider. Functional stool testing (like a GI-MAP) can help identify bacterial imbalances, infections, or digestive insufficiencies contributing to symptoms.
The Functional Medicine Takeaway
Constipation is your body’s way of signaling an imbalance. Rather than masking the symptom, functional medicine works to uncover why it’s happening, whether it’s stress, sluggish bile flow, thyroid dysfunction, or a microbial imbalance, and uses nutrition, lifestyle, and targeted therapies to restore balance naturally.
Your digestive system thrives when supported holistically, through hydration, mindful eating, nervous system regulation, and liver and gut care. True healing begins when the root cause is addressed, not just the symptom.
References
Camilleri, M., Bharucha, A. E., Farrugia, G., & Lembo, A. (2017). Functional constipation. Nature Reviews Disease Primers, 3, 17095. https://doi.org/10.1038/nrdp.2017.95
Müller-Lissner, S. A., Tack, J., Feng, Y., Schenck, F., & Specht Gryp, R. (2017). Levels of satisfaction with current chronic constipation treatment options in Europe – An internet survey. Alimentary Pharmacology & Therapeutics, 45(5), 637–648. https://doi.org/10.1111/apt.13917
Quigley, E. M. M. (2019). The gut microbiome in health and disease. Gastroenterology & Hepatology, 15(3), 143–155.
Tack, J., & Drossman, D. A. (2017). What’s new in Rome IV? Functional GI disorders: Disorders of gut–brain interaction. Gastroenterology, 150(6), 1257–1261. https://doi.org/10.1053/j.gastro.2016.10.031